Anne Main leads debate on the future of pharmacies
Anne leads a debate about the role that community pharmacies can play in an integrated health service.
I beg to move,
That this House has considered pharmacies and integrated healthcare in England.
It is a delight to serve under your chairmanship, Mr Bailey. In the light of the extreme pressures on our health services, particularly in the winter months—much has been made of this recently in the media, although it is not dissimilar to many other years—with our over- burdened frontline services, clogged up A&E departments and congested GP services, I believe it is vital that we explore new models of delivering patient care, particularly an integrated model of patient care.
In 2016, there was an average of 2,500 more attendances at major A&Es a day compared with 2015, which is a 6% increase. People aged 80-plus have the highest rates of A&E attendance. As a country, compared with only a few decades ago, we are now fortunate enough to benefit from innovative drug treatments, greater survival rates from complex surgery, better nutrition and better education; but, as a population, many of our residents are living longer. For example, in my constituency of St Albans, the average life expectancy for a pensioner is over 89 years—it is nearly 89 and a half years. However, for far too many of our constituents, the latter part of their lives brings a prolonged period of frail health, with dementia and diabetes on the rise and an increased incidence of ill health linked to lifestyle choices such as lack of exercise, alcohol, obesity and smoking. That period at the end of our lives is often not characterised as a period of good health.
We need to come up with a seamless, flexible model that makes the best use of precious resources and benefits patients. It is therefore timely to explore in this debate the role that local pharmacies play in local health services and the potential role that they might play to ease the strain on more congested frontline services. I also want to make the Government aware of the continuing importance of pharmacies in communities and their potential to do so much more.
In an ever-changing world, we have a duty continuously to challenge the old models of health delivery systems. In October, the Government proposed to reallocate money towards NHS frontline services. We all accept that the NHS is labouring under huge financial pressures, so any areas in which precious resources are dissipated due to inefficiencies or duplications ought to be considered. It is important to integrate community pharmacies into the NHS urgent care system and GP services. We need to promote a pharmacy-first culture for minor ailments to take pressure off frontline services.
Community pharmacies currently see some 1.6 million people a day in the UK. It is worth noting that the recent standard patient experience report for the East of England Ambulance Service NHS Trust in 2016 showed that 0% of respondents in my county of Hertfordshire had contacted a walk-in service, an out-of-hours GP service or a pharmacy service before contacting the ambulance service. I think we can agree that a lot more can be done to take the pressure off emergency frontline services.
Pharmacies are the most accessible health services in most communities: they are found on high streets, in supermarkets and in shopping centres. In St Albans, we have some great independent local pharmacists who want to get more involved and we even have the headquarters of the National Pharmacy Association, which supports independent pharmacies and helps them grow their businesses. We need to look at the current pharmacy model. In St Albans, patients can choose from five dispensing pharmacies within a half-mile area of the high street. Some pharmacies are just over the road from each other, and some have only yards between them. Given the Government’s financial support of £25,000 for those dispensing 2,500 prescriptions per annum, which comes directly out of our NHS budget, it is easy to see why we need to look at the model of provision and ask how we can get a better bang for the NHS buck.
I accept the Government’s assertion that a balance must be struck to ensure that pharmacies remain accessible but are not excessive in number and, importantly, that we have a range of offering. All the local pharmacies on the high street in St Albans are closed on Sunday, whereas the big supermarket pharmacies are open, in line with their shopping experience. It is worth noting that Sunday is the busiest day for most A&E services. However, a recent survey showed that 50% of people prefer, for a variety of reasons, not to use a pharmacy in a supermarket, particularly the retired, the elderly and other frequent pharmacy users. We therefore need to examine the model of opening hours, as well as location and the type of provision on offer. Given that many supermarkets are located outside the town centre, their pharmacies are not accessible to everyone, particularly the most vulnerable in society. Diversity and accessibility of provision are key to integrating pharmacy and health services.
Let us explore what pharmacies could do. Pharmacies should be capable of providing general health services. They could increasingly work beyond the traditional role and offer services to promote sexual health, increase physical wellbeing and give advice on flu immunisations and drug-harm prevention, for example. However, if we expect pharmacies to do more, we need the funding formula to reflect the quality of service they provide. That is what the pharmacies want. Local pharmacists in St Albans believe that they should be the first point of contact for advice on medicines, minor illnesses, healthy living and wellbeing. To facilitate that, the Quadrant pharmacy in St Albans has undertaken a major refit, with a brand new consulting room, and invested heavily in technology, including an expensive automated robot for dispensing medicine.
I visited the Quadrant—I am sure that many hon. Members made similar visits after the Government’s pronouncements in October—in November last year to discuss the opportunities and challenges facing small independent pharmacies. The pharmacy is a friendly, attractive place to pop into and is well-regarded by local people. It has the potential to do so much more, but that extra service does not come without a cost. If people spend time talking to their local pharmacist, the pharmacy gains nothing if they then walk out of the door and go off to see their GP. It is important that we recognise the role pharmacies are being asked to play in giving advice, holding consultations and, potentially, dispensing services. There must be some reflection of the cost involved in the staff time that it takes to do those things.
Rachel Solanki, the director of the Quadrant pharmacy, told me:
“General Practice will need to continue to be the gate keeper of referral to secondary care.”
However, she helpfully suggested
“a whole raft of services and support for self-limiting and long-term conditions”,
such as dealing with uncomplicated urinary tract infections in women, impetigo and bacterial skin infections; managing non-complex patients with high blood pressure; performing healthy heart and cholesterol checks; and supporting patients diagnosed with diabetes. The list was quite exhaustive. She proposed that pharmacies could and should act as wellbeing hubs for the communities they serve. She went on to say:
“The community pharmacist, a highly-skilled and trained individual, is the most accessible healthcare professional and is available without an appointment. If a mechanism could be found to incentivise and remunerate, we are confident the mutual agendas would be achieved.”
That is her view, and that of many other local pharmacists. There is a mutual agenda for providing good healthcare for patients that could be achieved if pharmacies were brought into play.
The Government’s proposals in October last year were a step in the right direction, but we need more detail. I want to ask the Minister a series of questions, and hopefully he will be able to answer some of them. How can the Government make smaller and local pharmacies more attractive and accessible for everyone? How can the Government encourage GPs to offload services such as flu jabs on to pharmacies? In saying “offload”, I recognise that where there is a cost to the pharmacy and the GP is in receipt of payment for that flu jab service, that needs to be considered, but I would like to hear the Minister’s views on that. How can the Government promote the pharmacy as an alternative local health provider that can be trusted and deliver a quality service? This is not just about having a shop that you take your prescription to and maybe pick up a few aspirin; it is about the pharmacy being a health provider. How can the Government increase pharmacy capacity to provide a broader range of health services and ensure the correct remuneration for the service provided?
Responding to an oral question on 2 March 2016, the then Health Minister, Lord Prior, stated:
“The big driving force going through healthcare and community pharmacy today is one of integration, which means that community pharmacies must in future work more closely with their local hospitals and GPs.”—[Official Report, House of Lords, 2 March 2016; Vol. 769, c. 817.]
That is the point of today’s debate. The Government have pursued several polices that are intended to lead to better integration of community pharmacies, including the introduction of a pharmacy integration fund as part of the 2016-17 community pharmacy settlement.
Last month, Richard Murray of the King’s Fund published a paper looking into the role of community pharmacies in the NHS. In December 2016, the Minister described that review as
“an essential road map that sets out how we are going to move the community pharmacy network away from a remuneration model based just on dispensing and on to services as well.”—[Official Report, 20 December 2016; Vol. 618, c. 1301.]
When can we expect a response to that incisive review?
The NHS “Five Year Forward View”, which was published in 2014, recognised that GPs are “under severe strain”, and many of us will have met GPs locally who have restated that view to us. It also states that steps will be taken to:
“Build the public’s understanding that pharmacies and on-line resources can help them deal with coughs, colds and other minor ailments without the need for a GP appointment or A&E visit.”
I urge the Government to listen to pharmacists when considering how to take that integration forward, as we do not want to lose what is good in the system, especially where it works well for our local patients. For example, I know that the Government are piloting an urgent medicine supply service. Rachel Solanki, the director of the Quadrant pharmacy, tells me that in Hertfordshire there is a local scheme that is so well regarded that it has now been rolled out again. Her concern is that the proposed national service does not necessarily promote a pharmacy-first culture. The Minister may wish to clarify that that is not the case, but that was the view she expressed to me. She was worried that there might be a perverse incentive to encourage patients to phone NHS 111 in order to get a referral to the pharmacy service.
In an email Rachel wrote to me recently, her view was that the change could have the unintended consequence
“of actually increasing NHS 111 calls for emergency medicines when they should be directed to community pharmacies first. Our local service offers both the facility to help the patients get their medicine but, more importantly; also offers incentivisation of the community pharmacy to promote ordering medicines in a timely way to reduce medicines waste, and hopefully therefore preventing a further incident of need.”
She thinks it unlikely that the proposed 111 service will operate both the services that we have locally and the new model, and she worries about losing the existing local scheme. Will the Minister reassure me by saying whether schemes such as the one operating in my county of Hertfordshire could still operate in tandem, or will they be mutually exclusive?
My hon. Friend is making a very powerful speech. Does she agree that although we must encourage clinical commissioning groups to work closely with community pharmacies—she has highlighted some good examples of that—the practice is patchy across the country? There is reluctance in some areas for clinical commissioning groups to engage with their local pharmacies. We have had that problem in York, where the CCG has been very reluctant to talk to local pharmacies. Local MPs, across parties, have written to it and finally got it to engage but it has been very slow, and we have to speed that up. We have great examples in some parts of the country, but poor examples in others.
My hon. Friend is absolutely right and completely backs up the point I was making. There is evidence of good practice but other areas could do much better. Without bringing pharmacies to the table and into the ongoing dialogue about this issue, we risk not having the new model that we would all like to see—one that operates consistently wherever people go.
There must be a consistent model in the drop-in pharmacy service that we are envisaging. Of course, people often use pharmacies away from where they live, such as where they work or when they are on holiday or visiting friends. If the model is patchy, as my hon. Friend says, the system will not improve and we will end up with a situation like the one that is found in many holiday towns. A few years ago, the Select Committee on Communities and Local Government looked into the fact that many seaside and holiday towns have enormous pressures on their frontline services. If something goes wrong when people are on holiday, although what happens is not necessarily catastrophic, they all end up at the local A&E services in hospitals. That huge problem was recognised, I think, in the 2006 seaside towns report by the CLG Committee. This is all part of evening out the stresses and strains on the system, which for many seaside holiday and tourist destinations are often huge.
Does my hon. Friend agree that that was largely the point of the Murray review, which she alluded to earlier? Integration throughout the whole of the NHS is vital, so that everybody knows what everybody else is doing and so that there are seamless pathways that everybody knows how to follow. That will ultimately give us benefits not only in pharmacies, but right across the NHS.
Absolutely. Rachel Solanki and her colleagues are not necessarily critical of change—that is important. Pharmacies are nervous about some of the things that may be coming along, but they are not critical of change. Indeed, they would welcome a debate on the innovative services that other pharmacies are operating around the country. The fact that we do not all know about these services in other places shows that there is not an integrated approach. The services include anticoagulation monitoring in Knowsley; medicines optimisation work for respiratory diseases in South Central; sexual health screening, including for hepatitis, syphilis and HIV, on the Isle of Wight; oral contraceptive supply in Manchester and other contraceptive provision in Newcastle; alcohol screening and brief intervention on the Wirral; healthy lung screening in Essex; pneumococcal immunisation in Sheffield; a reablement service on the Isle of Wight; and phlebotomy services in Coventry and Manchester. That is a long, diverse list of services that are provided by pharmacies in those areas.
Will my hon. Friend recognise that some innovative things are taking place in the west country, especially in my constituency?
I am happy to acknowledge that some fabulous things are happening in the west country. That list was given to me. I make no excuse for the fact that I thought it seemed fairly long already, but I am certain that there are a lot more services that hon. Members do not realise are out there—perhaps even in pharmacies in their own constituency or the one next-door that they go shopping in or visit with their families. The fact that we do not know about them shows that there is no integration in the system. We should be aware of it if these services are being rolled out. Perhaps there should be a directory that we could consult to find out what is going on in certain areas.
That list shows hon. Members the exciting possibilities that could be open to pharmacies, including those in the west country that were just referred to, if we just gave them the chance to embrace them. Rachel, the director of the Quadrant pharmacy, ended her observations with a positive endorsement of the “Community Pharmacy Forward View”. She told me that it has
“been developed and signed up to by all national community pharmacy organisations about the types of services that either need to be commissioned at a national level or pressure put on Sustainable Transformation Plans (STP) leaders locally to commission a service package to patients”.
My hon. Friend the Member for York Outer (Julian Sturdy) said that there is reluctance in some areas to embrace this. We need a strong steer from the Government that this is where we are going and that they had better wise up, get around the table and come up with a suitable model.
My hon. Friend is making an excellent point and I congratulate her on securing this debate. I have discovered the same thing as my hon. Friend the Member for York Outer (Julian Sturdy) in Suffolk. It is about trying to get the CCG to talk to the pharmacists. The interest of the NHS is our interest—it is a national interest—and not that of acute hospitals, the primary care sector or any particular sector. The NHS must operate in the national interest, and if that means involving pharmacists much more heavily and that we have to be the ones pushing for innovation, it is our job to do that.
My hon. Friend is absolutely right. I shall conclude my remarks soon, because I know that other hon. Members want to take part in this debate. If there is resistance in the system, I ask the Minister to find out what can be done to sort that out. How aware is he of resistance in the system? How much input have pharmacies had into highlighting what they would be prepared to do and their concerns about the fact that they are sometimes not being listened to in this debate? There seems to be broad agreement in the NHS “Five Year Forward View”, the “Community Pharmacy Forward View” and at the King’s Fund that the integration of pharmacies into NHS healthcare is the direction of travel.
The hon. Lady is making a really interesting speech. I have had such a big postbag on this issue because of the threats to pharmacies in my constituency. The fact that local community pharmacies are facing cuts is threatening the level of healthcare that people receive, particularly elderly people who cannot drive, people with children who need to be able to pop in with them after school and people with mobility issues. The cuts imposed by the Government are threatening the quality of the service that is being delivered. They need to address that before they look at further integration.
I agree that there are concerns. As I mentioned earlier, there are five dispensing pharmacies within half a mile in St Albans. Some are literally over the road from each other, although I know that model is not repeated everywhere. None of them is open on a Sunday and the only pharmacy that is open is in a big out-of-town superstore. We need to look at a model that addresses their proximity to the populations that need to use them and the hours that people are looking for pharmacies to be open. It is no good if people can access the seven-day-a-week pharmacy service only by getting in their car and driving two or three miles out of town. It is all part of the same thing.
That is why I support the point made in the Government’s proposals in October about models such as the one in St Albans, although this is not the case everywhere, where there are the big boys and smaller independents all in the same area. If the hon. Lady were to walk into Boots in my constituency—I have nothing against Boots, which is one of the pharmacies on my high street, as on many others—she could pick up sandwiches for her lunch, as well as a variety of health and beauty products, perfumes and so on. It is a one-stop shop for many things, a bit like a supermarket.
My concern is that we must not lose community pharmacies such as the Quadrant, which is a single pharmacy in a small shopping precinct that many people walk to and use locally. We have to have a balance of availability and opening hours. If we are truly to embrace an integrated system, some pharmacies may need to consider their opening hours and sign up to being open when they would not normally be. They will have to be remunerated for that as well. We need to look at the whole model. I understand that there are concerns, but our current model cannot continue. I want integration, and I want more money and more services directed towards pharmacies to make them viable and to make them the first hub for the community.
There is broad agreement that the direction of travel we need is towards getting people to use the most accessible health provider, which is the local pharmacy. That would keep many smaller pharmacies going. They cannot compete with all the other offerings from supermarkets such as Sainsbury’s, which has a pharmacy in its out-of-town store in London Colney, so we need to ensure that they compete as health hubs.
I look forward to hearing what the Minister has to say about these issues. I am sure that many other Members will make contributions about their local models, because the provision and the pharmacies on offer vary throughout the country. I accept that, in areas such as mine, the current model cannot continue, particularly if it asks for NHS funding, but we must not throw out the baby with the bathwater. I ask the Minister to say what more the Government will do to ensure that pharmacies have a real role in the integrated health service.
And at the end of the debate
This has been an excellent debate. I echo the Minister’s sadness about the fact that the two Opposition Members who made interventions did not stay for the whole debate. Unfortunately, some did not even arrive for the beginning of the debate, let alone stay for it all. That is disappointing, because this issue has filled my postbag and this debate is timely. There has been a lot of news about whether the NHS is under massive strain now more than ever. The reality is that we need a new model of working. Many hon. Members have put forward positive suggestions and have obviously been engaging with their local pharmacists. I am pleased that so many Government Members have made that effort and are so knowledgeable about their pharmacies.
The very fact that many private independent pharmacies like Quadrant have put money into their businesses—the hon. Member for Burnley (Julie Cooper), who leads for the Opposition, stressed her role in that—shows that there is a private model that can work with the NHS. It shows that those two models can be mutually beneficial and can learn from and give to each other. I am delighted that the Minister said that the emergency prescription system would not necessarily rule out the excellent system that Quadrant pharmacy operates, and I am delighted that we will soon hear the response to the Murray review, which contains many positive aspects about the way forward for pharmacies.
I am glad that there is so much consensus that keeping the model in which small, private independent pharmacies support the public NHS is an excellent way forward, and long may it reign. I am just concerned that we must ensure that small independent pharmacies in rural areas like the one that my hon. Friend the Member for Bury St Edmunds (Jo Churchill) represents are supported, perhaps with a weighting system. It is hard for them to compete with the big boys on the high street and the concessions in out-of-town supermarkets with parking and Sunday opening. I am glad that the Minister has been so frank with us, I am glad that there is so much consensus, and I am really looking forward to a great future for the NHS.
DISSOLUTION OF PARLIAMENT
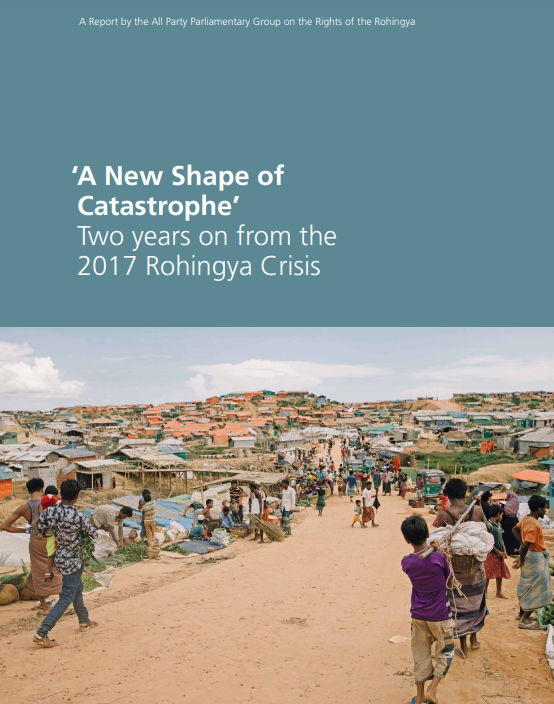
Watch: Anne Main, chair of the All Party Parliamentary Group on Bangladesh, talks about the Rohingya crisis and urges support for @DECappeal pic.twitter.com/FFL0lq8O0A
— DFID (@DFID_UK) October 12, 2017